NEUROLOGY Q&A
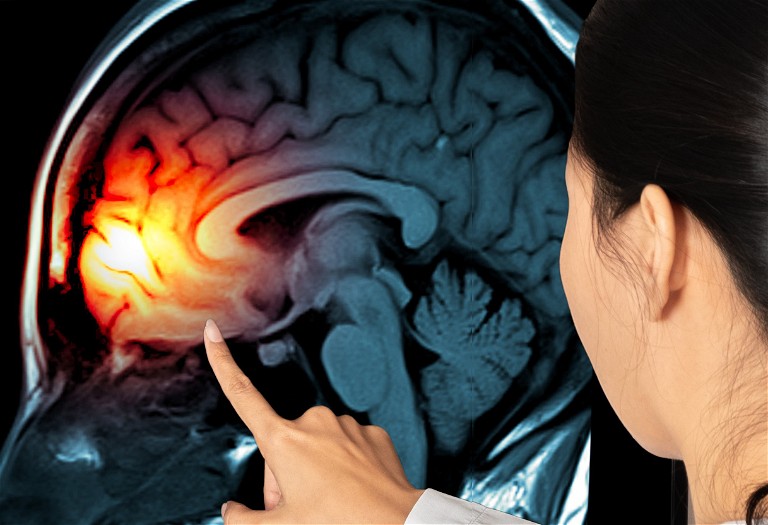
The importance of treating TBIs early
Christian Wandersee and John Stover from Vasopharm talk to Pharmafile about the effects a Traumatic Brain Injury (TBI) can have on a patient, as well as the need to focus on treatments in the acute stage of a TBI
Pharmafile: Why is TBI an important field?
Christian Wandersee: TBI is a leading cause of death and disability among young adults worldwide. The tremendous socio-economic impact is highly relevant to any society.
In the US alone, head trauma is the cause of approximately 2 million emergency room visits annually, 475,000 hospital admissions, nearly 52,000 deaths, and around 80,000 cases of severe long-term functional, cognitive and learning disabilities. Direct costs attributed to the current symptomatic treatment of TBI exceed $10bn per year in the US alone.
In Europe, 2.5 million people suffer a TBI annually, resulting in 1 million hospital admissions and 75,000 deaths. Overall, while TBI is the leading cause of death and disability in young adults, incidences in elderly patients are increasing. In younger patients, road traffic accidents are the most frequent cause of injury, with falls being most common in older patients. Moderate and severe head injury are associated with a 2.3- and 4.5-times higher risk of developing Alzheimer’s disease, respectively.
What is the unmet medical need in TBI?
John Stover: TBI is a form of brain injury that results from impact to the head or brain from an external translational, rotational, or combined force. This damage can impair cognitive, physical and psychosocial functioning temporarily or permanently. Such long-term impairment can lead to disability and loss of independence. In addition to acute changes that dominate the initial phase of injury, persisting alterations will impair improvement years after the initial injury. Current approaches to the symptomatic treatment of acute TBI during the acute phase focus on simple aggressive measures to increase blood pressure and reduce intracranial pressure. This hopes to limit long-term physical and cognitive defects. Additional specific treatment is needed to reduce increases in intracranial pressure, thereby decreasing the aggressiveness of current treatment options.
There is a strong need for a specific treatment to reduce the extent and duration of key pathologic processes of TBI. The successful control of activated key pathologic processes will support and facilitate subsequent improvement. In this context, decreasing the production of nitrate radicals is a defined specific treatment known to prevent structural damage and functional impairment. This in turn promotes progressive regeneration, thereby mitigating the suffering from mid-to-long term consequences of TBI.
What do clinicians need to treat TBI patients more effectively?
Christian Wandersee: Treatment of TBI patients involves two components: the acute phase and the recovery phase. In the acute phase, the priority is patient survival and stabilisation, whilst the recovery phase is more directed towards rehabilitation and recovery of function. Clinicians would like to see a drug that shows a positive effect during the acute phase, reducing the risk of secondary damage and decreasing elevated intracranial pressure. If early stability can be achieved with less aggressive, basic treatment interventions, improved neurologic function would be achieved by attenuating early inflammatory processes and mitigating subsequent flares in local neuroinflammation. For physicians, it is crucial to achieve an improved clinical and neurologic condition during the acute phase, for this will positively impact later improvements as patients transition from the acute to chronic phase.
A specific pharmacologic target is needed to create a better baseline condition during the acute phase after TBI, helping make the already injured brain less vulnerable to additional insults. Such an improved condition will enhance the future progress in neurologic recovery. This will address the current frustration felt by physicians due to the lack of a specific neuroprotectant drug.
What is typical for the early phase of TBI?
John Stover: The acute phase of TBI is dominated by an excessive activation of many different, predominantly inflammatory processes, which are no longer subject to their regular control mechanisms. As a consequence, the initial damage will progress over time, exacerbating subsequent neuropsychological and cognitive impairment typical in patients with moderate and severe TBI.
During the early phase, it is important to avoid further brain damage related to metabolic deterioration, low blood pressure, decreased oxygen supply and activated inflammation. In principle, the acute phase determines survival, and the level of impairment in the surviving patients.
What is typical for the late phase of TBI?
Christian Wandersee: The late phase expanding over weeks to months is dominated by recurrent inflammation and infections as well as progressive structural and functional decline, which hinder neuropsychologic improvement. In general, the late phase determines the extent of recovery.
Why should we focus on the early phase of TBI?
John Stover: We must stabilise the patients as early as possible after TBI to reduce the extent of brain damage during the early phase. This early control is critical to create a basis that allows improved recovery over time. The impact of effective treatment in the first hours and days following the trauma will manifest throughout the rest of the patient’s life.
What makes Vasopharm’s TBI treatment so exciting?
Christian Wandersee: Ronopterin is characterised by a well-defined mechanism of action. It mimics an enzyme-specific co-factor that inhibits the activated and upregulated inducible Nitric Oxide Synthase (iNOS). Inhibiting iNOS prevents excessive synthesis of nitric oxide and derived toxic molecules (nitrate radicals) known to induce substantial brain damage. In addition to its activation in resident brain cells (astrocytes, neurons, microglia), iNOS is also expressed in invading cells (neutrophils, macrophages) as part of the activated local and systemic inflammatory cascade. This activation and expression profile defines the specific treatment needs of inhibiting iNOS early during the acute phase.
John Stover: Ronopterin has the potential to be the first successful drug therapy for TBI with meaningful improvements in neurologic outcome and reduction in aggressive treatment options. Ronopterin has successfully passed three clinical trials. The results obtained in the two TBI trials show that Ronopterin significantly reduces glutamine in brain microdialysis, decreases aggressive critical care, and improves neurologic outcome as well as quality of life after moderate and severe TBI, particularly with early infusion within 12 hours after injury.

Christian Wandersee is a co-founder of Vasopharm. He joined the company in 1999. From January 2000 to July 2004, he served as Managing Director and CFO. In August 2004, he became CEO of the company.

Prof Dr John Stover joined Vasopharm in 2021 as acting CMO. He worked for more than 15 years in the fields of intensive care medicine and neurosurgery at the University Hospital Zurich, Switzerland; Charité Berlin, Germany; Henry Ford Hospital, Detroit, and University of Pennsylvania, Philadelphia, US. Afterwards, he acquired nine years of experience in Clinical Research and Development as well as Medical Affairs at Fresenius Kabi, Germany, Vifor Pharma, Switzerland, and Alexion Pharmaceuticals, Switzerland.