CARDIOVASCULAR & METABOLIC
Taking action to address Europe’s non-communicable disease epidemic
Stefan Woxström at AstraZeneca considers the high rates of non-communicable diseases and how governments and healthcare systems can improve their treatments
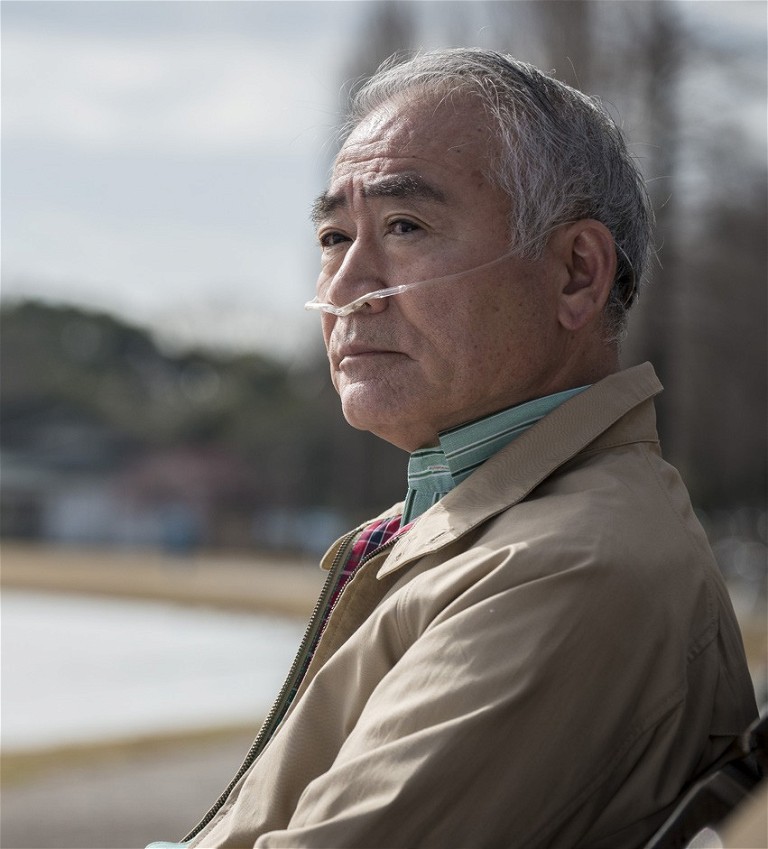
Across Europe we’re facing a health epidemic of unanticipated proportions, one that threatens the sustainability of our health systems, the well-being of our populations and the prosperity of our societies. Non-communicable diseases (NCDs) are now the leading cause of mortality and morbidity in Europe, responsible for over 90% of deaths across the region. Rates of NCDs are expected to rise even further in line with ageing and growing populations and because of new health risks linked to climate change.
NCDs, such as chronic cardiovascular, respiratory and kidney diseases, account for the largest part of many countries’ healthcare expenditure (often as high as 25%), as well as leading to societal costs incurred through loss of productivity and workforce. With governments across Europe struggling to manage the escalating health and financial burden of NCDs versus competing priorities and ongoing repercussions from the COVID-19 pandemic, an optimised, forward-looking approach to NCDs is needed to reduce costs and inefficiencies in care.
Bringing policy attention to NCDs
Although disease-specific policies for NCDs are very much in their infancy, we are starting to see greater investment and policy action to target NCDs across Europe. For example, the Healthier Together – EU NCD Initiative, which was adopted by the European Commission in 2021, plus the ongoing work by the European Parliament Subcommittee on Public Health (SANT) to develop a report with specific policy recommendations to tackle NCDs and improve the quality of life of European citizens.

As we consider how to address the growing burden of NCDs, there are a few priority areas that will help Member States to drive change and make progress towards the Sustainable Development Goal to reduce premature mortality from NCDs by one-third by 2030.
“Non-communicable diseases are now the leading cause of mortality and morbidity in Europe”
Acting earlier to reduce the burden from NCDs
Nearly 80% of European healthcare costs are spent on managing NCDs – often when it’s too late to change disease prognoses – compared to less than 3% that is allocated to disease prevention. Health promotion and disease prevention interventions can reduce the prevalence of NCDs by as much as 70%, yet despite their relative low cost, many European health systems continue to underserve those who are at risk of potentially life-threatening conditions. For many governments, primary prevention remains their greatest focus, however considerable benefits and savings can also be achieved through secondary prevention, demanding policy attention and action throughout the entire disease pathway.
Furthermore, the benefits achieved from earlier detection of disease expand far beyond patients and healthcare systems – it is also good for the planet as a healthy patient is a greener patient. New technologies, such as artificial intelligence (AI), are now being applied to accelerate NCD detection, helping to ensure that patients can receive the care they need at the earliest opportunity. The NHS is trialling AI to interpret echocardiogram images, helping to detect heart failure earlier, with a goal to improve patient outcomes, reduce the need for hospitalisation/ambulatory care and ultimately lower healthcare-associated carbon emissions.
Embracing a disease-specific approach to NCDs
While there are general principles that apply to all NCDs, differences in causality, prevalence, impact and available solutions for detection and management mean that taking a holistic approach may not always adequately reflect the individual needs and burden posed by each disease.
As an example, chronic kidney disease (CKD) is among the NCDs with the highest unmet need in Europe, affecting 100 million Europeans with another 300 million at risk – ahigher prevalence than diabetes and cancer combined. Although low-cost and easily administrable tests are widely available, around one-third of people with severe CKD do not know they have the disease, which if left untreated can lead to severe illness and death at an annual cost of approximately €140bn to governments across Europe. Despite this, CKD is not considered a ‘major’ NCD and is often overlooked by policymakers.
CKD should be considered a condition in its own right; however, it is also closely comorbid with other conditions such as hypertension, diabetes and heart disease. Where NCDs are closely linked, huge gains can be achieved by providing integrated care. If Member States introduce targeted health checks of high-risk individuals who present with the main shared risk factors and comorbidities, there is an opportunity to improve management, reduce complications and save downstream costs for healthcare systems across Europe.
Fostering innovation to improve disease outcomes
Advances in innovation have been instrumental in developing novel interventions for NCDs that not only alleviate symptoms but can stop or even reverse disease. Scientific innovation has great potential to shift us from today’s treatments to tomorrow’s cures, fundamentally changing the outlook and prognosis for many NCDs. However, to make these advancements a reality and promote a healthier Europe, we must ensure that the regulatory environment encourages progress.
The EU is currently working to reform its European Pharmaceutical Legislation – the most significant overhaul of EU health law in the last two decades. The goals to prevent drug shortages and ensure timely, equitable access to safe, effective and affordable medicines are undoubtedly critical. However, it is essential that the proposed changes continue to encourage the development of cutting-edge scientific and technological medicines in Europe. We’ve already seen a decline in R&D investment across the region, with Europe now conducting half as many clinical trials as the US and a third of those in China. This is having a direct impact on patient care, with just one in five new medicines now originating in Europe.
With such considerable unmet need in NCDs it is essential that Europe fosters a favourable infrastructure for R&D, where biopharmaceutical innovation is embraced and appropriately valued. The ongoing work from the SANT Committee highlights that innovation in the development of technologies, medicines and healthcare practices will be crucial to address preventable risk factors and find new and better treatments for NCDs. By continuing to invest in R&D, European healthcare systems will be able to evolve and develop faster, accelerating the provision of novel therapies for patients across the region and worldwide.
“ Now is the time to join together to implement effective policies and actions to reduce the burden of major NCDs and improve population health and well-being ”

Collaboration to advance NCD care
Addressing the growing burden of NCDs and ensuring the sustainability of Europe’s healthcare systems will demand a coordinated response from all stakeholders involved in the provision of care. More needs to be done to improve data collection and consolidate research on the prevalence and value of early intervention in NCDs, particularly for comorbidities, which are currently under-explored. Sharing evidence-based best practices between European Member States will be key to adopting effective prevention measures and innovative practices for NCDs.

Recognising the need for greater connection on this issue, the Partnership for Health System Sustainability and Resilience (PHSSR), a global collaboration that involves academic, non-governmental, life sciences, healthcare and business organisations, has established an EU Expert Advisory Group to make recommendations to European institutions on how they can support the sustainability and resilience of healthcare systems across the region. Their first policy report, expected to be launched in late 2023, will focus on ambitious measures to drive practice change on NCDs across Europe.
For too long NCDs have not received enough attention. Now is the time to join together to implement effective policies and actions to reduce the burden of major NCDs and improve population health and well-being.

Stefan Woxström is senior vice president of AstraZeneca Europe and Canada (EUCAN), responsible for leading the company’s sales, marketing and commercial operations across 30 countries. Working from the EUCAN Headquarters in Baar, Switzerland, Stefan is expanding AstraZeneca’s therapy areas across the region and transforming healthcare delivery to achieve the greatest benefit for patients, healthcare systems and societies.