ANTIMICROBIAL RESISTANCE
Resisting change: The pathway to better AMR planning
The latest global survey on antimicrobial resistance has seen a global plan initiated by WHO. ICON’s Caroline Forkin talks us through the various actions that should be taken to improve AMR planning
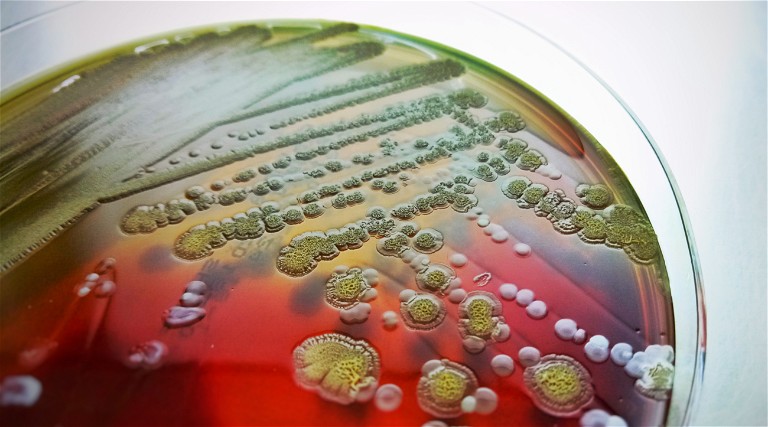
Antimicrobial resistance (AMR) is an urgent and growing public health threat. Since the transformative global adoption of antimicrobials in the last century, pervasive misuse and overuse has driven widespread AMR in pathogens, and rendered once reliable treatments ineffective. The drivers of AMR are multifaceted, with far-reaching consequences. Meanwhile, the development of alternative antimicrobials and interventions has been slow. With so many forces accelerating a problem that spans the globe, mitigation will require unprecedented social support, and coordinated, holistic action is needed to help combat the growing global public health crisis of AMR.
Reinforce understanding of AMR
Many antimicrobial drugs already have an ancient history of use and evolved resistance by microbes. Understanding the evolutionary relationship between antimicrobials and microbial resistance helps explain why acquired AMR can emerge so quickly following intensive antimicrobial use.
Microbial resistance is the result of a random genetic mutation or a combination of mutations impairing an antimicrobial’s utility. In the absence of an antimicrobial, resistance mutations tend to be disadvantageous because they are costly. However, when a population is exposed to antimicrobials, resistance mutations are often necessary for survival, and are likely to be passed from one generation to the next. Resistance genes can also be spread between unrelated microbes through horizontal gene transfer (HGT).1
Because the presence of antimicrobials determines whether resistance mutations provide a competitive advantage or disadvantage, AMR prevalence is tightly correlated to the likelihood of antimicrobial exposure. Before widespread antimicrobial use by humans, AMR was generally contained to a small population of microbes that had natural, sustained exposure to an antimicrobial. However, when an antimicrobial is intensively applied by humans, the advantage of acquiring resistance becomes widespread.2
Following sustained antimicrobial use in a clinical or agricultural setting, pre-existing resistance genes – which took generations of antimicrobial exposure to first evolve – can be rapidly and ubiquitously acquired through HGT by microbes in a shared environment. Microbes transported to other environments may then bring resistance with them.
Understanding AMR mechanisms is key to developing intervention strategies to disrupt AMR emergence and spread. In addition, comprehending why AMR occurs, and the risks it poses to public health, will support personal investment in initiatives to combat it.
Optimise antimicrobial use
The utility of antimicrobials in preventing infectious disease has transformed medicine and agriculture. Preventative antibiotics drastically reduced the risk of surgery, and common deadly diseases, including pneumonia and tuberculosis, suddenly became treatable. Moreover, antibiotics in agriculture made it possible to raise faster-growing livestock at higher densities.
Initially, the application of antimicrobials in these settings was indiscriminate.3 However, the subsequent body of evidence linking antimicrobials to AMR motivated private initiatives and governmental regulations to temper antimicrobial use. Still, substantial progress must be made before antimicrobial application is optimised in healthcare and food production.
Healthcare: Up to 50% of all antimicrobials may be being used inappropriately in human healthcare. 4 Appropriate and restricted use of antimicrobials will require the implementation of diagnostics able to indicate which treatment is most likely to be effective, and reduce the number of antimicrobials prescribed. Diagnostics that can monitor a patient’s response to treatment may also help to prevent continued use of an ineffective treatment. Eventually, the adoption of treatment alternatives to existing antimicrobials may help ensure treatment efficacy when the risk of AMR is high. Optimised antimicrobial use also depends on patient compliance. Suspending treatment before an infection is entirely cleared can lead to a recurrence that is more resistant than an initial infection, and can increase the risk of AMR outbreaks. Here, clinicians play a critical role in educating patients about the importance of following an antimicrobial regimen.
Food production: Agriculture accounts for more than 75% of annual antimicrobial consumption in the EU and the US, and has been directly linked to AMR disease in humans. 5 Addressing overuse and misuse of antimicrobials in agriculture will involve three strategies:
1. Abolition of trace antibiotics used in feed to promote growth
2. Abolition of continuous low-dose antibiotics for disease prevention
3. Using alternative antimicrobial treatments wherever possible
Antimicrobials also enable unhealthy agricultural practises promoting disease acquisition and transmission, such as overcrowding and inbreeding. Reintroducing practises that promote the health of livestock and crops could help reduce the number of infections, and help to minimise the need for preventative antimicrobials.
Governmental policies and initiatives supporting more sustainable food production practises can have a profound effect on optimising antimicrobial use in agriculture. For example, Vietnam’s National Action Plan for addressing AMR prompted the ViParc (Vietnamese Platform for Antimicrobial Reductions in Chicken Production) project. ViParc became the first large-scale intervention tackling antimicrobial overuse in Southeast Asian animal production systems.6
ViParc offered small-scale poultry farms in Vietnam’s Mekong Delta veterinary care as an alternative to antimicrobials. The project determined that access to trained veterinarians reduced antimicrobial use by 66%, in a region where food production accounted for 72% of use overall.7
Prioritise disease prevention
The risk of AMR emergence and transmission is especially acute in low-income countries and disadvantaged communities. Social and economic issues, especially overcrowded living conditions, unsanitary water, and limited healthcare access, increase the risk of acquiring and spreading AMR disease.8 Reducing the incidence and spread of infectious disease in communities most vulnerable to AMR infection will be critical to combatting AMR.
Investments in public health resources may be even more effective with appropriate communication, awareness, and training, to promote understanding of AMR prevention. Informing healthcare and food production workers about the risk of antimicrobial overuse, and training them in measures to prevent contracting and spreading AMR disease, will help to prevent transmission from AMR hotspots to surrounding communities. Campaigns that engage a public audience, such as World Antimicrobial Awareness Week, are also key to encouraging awareness and best practises among the general public, health workers, and policy makers.
Establish funding for AMR research and development
While the problem of AMR has snowballed, the development of new antimicrobials has slowed. The incentive for pharmaceutical companies to develop new antibiotics is especially low, because antibiotic efficacy declines over time, and the upfront cost of drug development has risen to 1.5 billion dollars.9 Implementation of financial incentives for pharmaceuticals may facilitate reduced reliance on traditional antimicrobials. The recent European Commission strategy document includes a programme to develop incentives for drug and diagnostic development, and marks the first time a major governing body has codified this approach.
Existing programmes for the funding of AMR research and development include the Global AMR Innovation Fund (GAMRIF), a UK-based group with the goal of reducing the threat of AMR in low- and middle-income countries. GAMRIF has a goal of funding the development of two to four novel antibiotics and making them available to patients by 2030. State and local initiatives to combat AMR may be further supported by national efforts, such as the Antibiotic Resistance Solutions Initiative funded by the Centers for Disease Control (CDC).
Development of cheap, effective, and accessible diagnostics
The development of rapid, accessible, and low-cost diagnostics would enable the timely use of targeted therapeutics, and allow clinicians to better monitor treatment effectiveness over time. One diagnostic method uses polymerase chain reaction (PCR) to identify pathogens by their genetic fingerprint to diagnose disease. This method is substantially faster than traditional culturing methods. PCR diagnostics enable clinicians to diagnose tuberculosis within hours instead of weeks following the collection of a clinical sample.10 However, PCR techniques require laboratory equipment and conditions that limit the technique’s application.
Adaptations of PCR technology, such as PCR Loop Mediated Isothermal Amplification (PCR LAMP), improve the practicality of PCR-based diagnostics by making them cheaper and transportable. The minimal equipment and speed of LAMP made it an ideal tool for rapid COVID-19 testing.11
Improving AMR diagnostics will require simplifying diagnostic workflows, taking advantage of technologies such as nextgeneration sequencing (NGS) and artificial intelligence (AI). Researchers at the Oxford Biomedical Research Centre (OxBRC) are working on a modern diagnostic platform using whole genome sequencing analysis that is scalable and open-source.12The diagnostics platform aims to assist in outbreak response, infection control, and direct patient care on a global scale. Another global support system, the CDC’s AR Lab Network, helps laboratories enhance detection of AMR using DNA sequencing technologies. 13
Developing alternatives to antimicrobials
Alternative treatment methods to antimicrobials include bacteriophages, probiotics, and vaccines. While all of these treatments have promise, vaccines may be especially impactful in the prevention of community disease spread and reduction of antimicrobial use in agricultural settings.14
Unlike response-based treatments that can select for the most resistant microbes in an exposed population, vaccines facilitate an immune response that is early, targeted, and varied between individuals. Microbes are less likely to develop resistance to vaccines than to other targeted treatments.15
However, until the COVID-19 vaccines, vaccine development was expected to take more than a decade. Now, vaccine development for AMR may be expedited by genetic sequencing technology, COVID- 19-informed models for accelerated clinical trials, and fast-tracked regulatory approval processes.16
Research into antimicrobial alternatives will benefit from establishing combination treatments and treatment cycling, helping antimicrobials maintain efficacy, especially when AMR spread is likely. Determining the real-world efficacy and optimal use of diagnostics and treatments requires organised monitoring and surveillance of AMR by dedicated organisations.
Coordinate surveillance and monitoring of AMR
Coordinating observations of AMR emergence and spread helps identify key drivers of AMR and effective prevention strategies that can inform preventative action plans. The Advisory Group on Integrated Surveillance of Antimicrobial Resistance (AGISAR) started the development of WHO guidelines on the use of antimicrobials in food production, and contributed a guidance document on integrated surveillance of AMR.17The Transatlantic Taskforce on Antimicrobial Resistance (TATFAR) was chartered by the EU and the US in 2009 to improve peer collaboration, information exchange, and understanding of best practises for contending with AMR. 18The Global Antimicrobial Resistance and Use Surveillance System (GLASS) outlines and facilitates standardised collection, analysis, interpretation, and sharing of AMR data to inform research. In 2021, 64,000 surveillance sites in 66 countries contributed data. Participation has grown exponentially since the system’s initiation in 2015. 19
Implement action plans
Governments and international groups have a pivotal role in developing and enforcing holistic action plans to combat AMR. The tripartite partnership of global organisations – WHO, the Food and Agriculture Organisation and the World Organisation for Animal Health – coordinated The Global Action Plan (GAP) to combat AMR in 2015, and encouraged countries to develop their own national plans.20The plan jumpstarted global initiatives such as GLASS, and the Interagency Coordination Group. 21
GAP has supported the development of national action plans to combat AMR in 144 countries. These national plans are well positioned to use insights from global AMR monitoring, and research efforts for locally tailored enforcement and multifaceted engagement strategies.22
Conclusion
AMR is a problem of daunting scope, and we need to be prepared for the next disease-X type global threat. However, the evolutionary mechanisms and consequences of AMR are well characterised and understood. There are concrete actions that individuals, institutions, and governments can take to address the drivers of AMR and treat AMR infection. Working in concert, actions from diverse players will make it harder for microbes to evolve and sustain resistance to life-saving treatments.
References
- Munita JM, Arias CA Mechanisms of Antibiotic Resistance, Microbiol Spectr; 4(2)
- Aminov RI, A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future, Front Microbiol, 1:134, 2010
- Kirchhelle C, Toxic Priorities: Antibiotics and the FDA. In: Pyrrhic Progress. The History of Antibiotics in Anglo-American Food Production. Rutgers University Press: pp54-74, 2020
- Milani RV et al, Reducing inappropriate outpatient antibiotic prescribing: normative comparison using unblinded provider reports, BMJ Open Qual, 8(1):e000351, 2019
- Boeckel TP et al, Global trends in antimicrobial use in food animals, PNAS, 112(18): pp5,649-5,654, 2015
- Carrique-Mas JJ, Rushton J, Integrated Interventions to Tackle Antimicrobial Usage in Animal Production Systems: The ViParc Project in Vietnam. Front Microbiol, 2017
- Phu DH et al, Reducing Antimicrobial Usage in Small-Scale Chicken Farms in Vietnam: A 3-Year Intervention Study. Front Vet Sci, 7:612993, 2021
- Rousham EK, Unicomb L, Islam MA, Human, animal and environmental contributors to antibiotic resistance in low-resource settings: integrating behavioural, epidemiological and One Health approaches, Proceedings of the Royal Society B: Biological Sciences, 285(1,876):20180332, 2018
- Plackett B, Why big pharma has abandoned antibiotics, Nature, 586(7830):S50-S52, 2020
- Cheng VC et al, Clinical evaluation of the polymerase chain reaction for the rapid diagnosis of tuberculosis. J Clin Pathol, 57(3): pp281-285, 2004
- Amaral C et al, A molecular test based on RT-LAMP for rapid, sensitive and inexpensive colorimetric detection of SARS-CoV-2 in clinical samples. Sci Rep, 11(1):16430, 2021
- Visit: oxfordbrc.nihr.ac.uk/research-themes-overview/antimicrobial-resistance-and-modernising-microbiology
- Visit: www.cdc.gov/drugresistance/solutions-initiative/arlab-network.html
- Allen HK et al, Finding alternatives to antibiotics, Ann N Y Acad Sci, 1323: pp91-100, 2014
- Micoli F et al, The role of vaccines in combatting antimicrobial resistance. Nat Rev Microbiol. 19(5): pp287-302, 2021
- Monrad JT, Sandbrink JB, Cherian NG, Promoting versatile vaccine development for emerging pandemics. npj Vaccines, 6(1):26, 2021
- Visit: www.agisar.org
- Visit: www.cdc.gov/drugresistance/tatfar/index.html
- Visit: www.who.int/initiatives/glass
- Visit: apps.who.int/iris/handle/10665/253236
- Inoue H, Minghui R. Antimicrobial resistance: translating political commitment into national action. Bull World Health Organ. 95(4): p242, 2017
- Munkholm L, Rubin O, The global governance of antimicrobial resistance: a cross-country study of alignment between the global action plan and national action plans. Globalization and Health, 16(1):109, 2020

Dr Caroline Forkin brings 26 years’ experience in clinical, pharmaceutical and global health settings, including extensive experience in Africa.
With a clinical background in Infectious Diseases, Caroline’s experience in Africa included senior roles as HIV/AIDS Advisor for both the World Bank and the Irish Government. These roles involved working with the Mozambican Ministry of Health, National AIDS Council, together with other global health entities such as the Clinton Foundation HIV/AIDS Initiative, the Global Fund for AIDS, TB, and Malaria, the President’s Emergency Plan for AIDS Relief. Dr Forkin’s pharma experience prior to joining ICON includes country medical lead for two biotech companies. Her role at ICON is Vice President for Clinical Research Services, with responsibility for all our studies in Africa and the Middle East.