ONCOLOGY
Supporting the challenges of innovative systemic treatments
Dr Stuart Hill, Medical Director, Merck UK & Ireland, highlights how the benefits of immunotherapy can be maximised to meet the needs of each and ever y patient
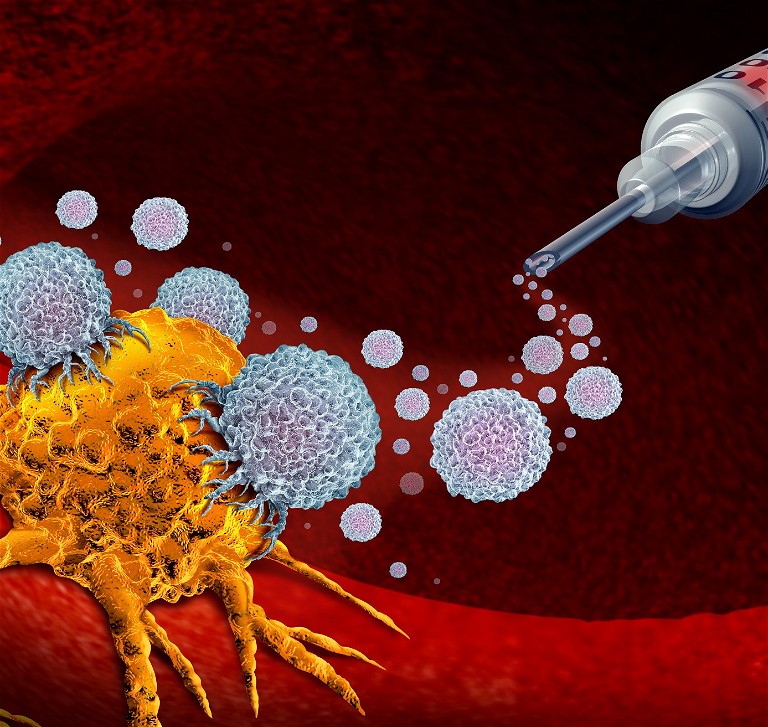
In recent years, we have seen significant innovation in the way that we treat cancer, as newer treatments such as immunotherapies, including CAR-T therapy and targeted therapies, have all brought with them a new set of challenges. These range from equity of access (stemming from practical issues around resources in hospitals hindering treatment delivery), to how best to manage complex immunorelated side-effects, and to the ongoing issues around biomarker testing. Many cancers have recently had new systemic treatments approved for use by the MHRA and recommended by NICE on the NHS, and brought to light these challenges faced by clinicians across the treatment pathway and throughout the healthcare system.
Service design adaptation is needed
As a result of the increasing number of patients being initiated on immunotherapies, for example, there is an increasing impact on overall clinic capacity. There aren’t suddenly more chemotherapy chairs and spaces that can be used to support these new treatments. Service provision and capacity needs to be addressed to accommodate the growing patient numbers. As more cancers are being treated with immunotherapy options, the number of patients treated with them will continue to grow. There is significant variance across the country on how service design is set up to support the provision of newer therapies – with some regions/models of care faring better than others.
There are also many ways immunotherapies are used, for example, as a single agent or as part of a combination treatment. This can also create challenges with the service capacity and timing of treatment. Patient experience also needs to be considered in terms of distance travelled to receive treatment, as well as the overall amount of time that they receive treatment.
While this will not change overnight, these issues need to be addressed and reviewed to ensure the potential benefits of immunotherapies can be fully unlocked. Although the pharma industry can’t necessarily offer support to improve service design, we have collaboratively worked with clinicians to bring to light the key challenges and needs, and will continue to do so. We’ve also raised awareness and understanding among key decision makers who can use the clinicians’ personal experiences to create solutions.
Biomarker testing is on the increase
In addition to service design and provision, we have seen an increased use of biomarker testing, which brings additional challenges across the UK in terms of speed of testing, lack of consistency in testing across the UK, and how testing is funded and positioned in the treatment pathway. These factors can impact how patients get the right treatment at the right time for their type of cancer. These challenges are not unique to any one tumour type, but are consistent across the board for immunotherapies, as well as the newer targeted therapies. Pharma has an important role to play in fully understanding the significance of testing, and in educating clinicians to ensure the best clinical outcomes.
Learning from clinical experience
We now have 10 years of follow-up data from the melanoma trials where immunotherapy was first used, and there is a clear long-term benefit of these treatments, including an increase in overall survival. All the lessons that we have learnt can be directly transferable to Genitourinary (GU) cancers, such as how to manage the side-effects, and how to best manage the treatment pathway and decision-making by the multi-disciplinary team. Whilst we’ve got to wait and see the long-term outcomes in other cancers, we shouldn’t assume that because it’s happened in one cancer type that it’s going to happen elsewhere. However, the data as it stands does potentially indicate a similar trend. Whilst we wait for long-term data, pharma has an important role in collating real-world evidence to support the use of immunotherapies, and to continue to inform clinicians on the benefits of these treatments, along with how to interpret the data that is continuing to emerge.
Support required for all in managing side effects
Managing the side-effects of immunotherapy is one of the biggest clinical challenges. Successful management is critical to both patient outcomes and the patient experience. Managing side-effects appropriately can only be done if there is an understanding across the wider clinical team of who may encounter a patient during treatment, such as A&E and acute care. There are many healthcare professionals (HCPs) who need educating on understanding the toxicities associated with immunotherapies, and appreciating that they are very different from chemotherapy, where they may have more knowledge and experience. There is an opportunity for larger teaching hospitals who have more experience, to help support smaller regional/district hospitals in helping manage side-effects appropriately. This specialist knowledge is something that is only acquired through experience, and it’s important to recognise that with any newer therapy, education is key to ensuring the best patient care.
How pharma can help
At Merck, we are committed to providing good quality information for HCPs. With innovation comes some form of challenge, and there is a need to ensure that information is provided to ensure the best possible clinical and patient outcome.
It is our duty as an industry to help support and provide guidance to HCPs, who are part of a treatment pathway on how to manage care with these new systemic treatments, and how to best deal with the complex needs of patients.
There is a focus on sharing best practice to support some of the themes already mentioned around service design to deliver the best care to their patients. With there being such variance across the country in the way that things are done, anything that we as an industry can do to help bring equity of delivery in the care pathway is important. At Merck, we have several initiatives working closely with HCPs to capture key learnings and best practice. These are developed into resources and content that are shared across different audiences, to help drive discussion and address some of the areas where improvements to patient outcomes can be made.
With any new treatment innovation, pharma is instrumental in ensuring that the right studies and research are conducted that inform important clinical decisions – proving that outcomes will last in the real world, as we’ve seen in clinical studies. It’s also important that we set up trial designs that are innovative and forward-thinking – looking at how to best maximise the benefit of immunotherapy, using them as single and combination agents across different tumour types.
We must also ensure speed of access so that patients get the treatments as quickly as possible. We have a responsibility, to those patients who may potentially benefit to work closely with regulators and funding bodies, to minimise the time in those processes to speed up access.
NICE’s Innovative Licensing and Access Pathway process, launched last year, is a step in the right direction. The initiative allows companies to work with NICE and the MHRA much earlier in the development process, receiving advice and input on clinical trial design, to ensure optimal data generation for both regulatory approval and health technology appraisal. This process should lead to quicker market access for companies, and faster access to innovative medicines for patients.
With companies and key stakeholders in healthcare systems coming together to align quicker in decision-making and benefitrisk, clinical outcomes for patients should ultimately be improved.
Looking to the future
Given the body of evidence that is still emerging in long-term use of immunotherapies, closely evaluating the data to make sure we are personalising treatment, and understanding the drivers of treatment efficacy, is critical. Irrespective of what the systemic treatment is, the only way we are going to be able to do the best for patients in the future is by identifying the right oncogenic drivers that are causing the cancer to grow and develop, so that we can target the right intervention to stop it.

Dr Stuart Hill is Medical Director, Merck UK & Ireland. In 2010, Stuart joined Merck and has worked for the last 10 years in the Oncology Business, which he has led as Business Unit Director for the last 3.5 years. The heavy focus on translating science into improved outcomes for patients has inspired Stuart to now take up the leadership of the Medical Affairs team for Merck’s UK & Ireland operation.